Peripheral IV Therapy:
Common Complications & Clinical Signs
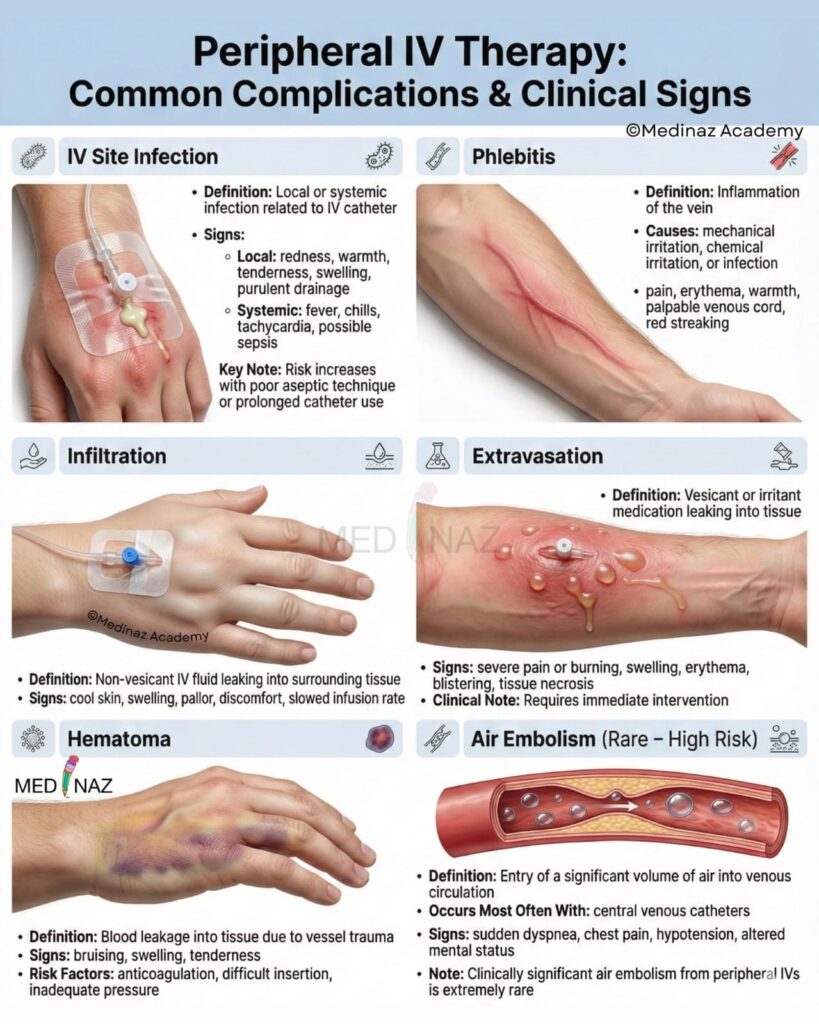
Peripheral IV Therapy: Common Complication & Clinical Signs
Peripheral intravenous (IV) therapy is one of the most frequently performed clinical procedures in healthcare settings. It is used for administering fluids, medications, blood products, and nutrition. Although peripheral IV therapy is generally safe, complications can occur if the site is not properly monitored or managed. Early recognition of complications and prompt intervention are essential to ensure patient safety and comfort.
This blog post discusses the common complications of peripheral IV therapy and their clinical signs, with a focus on practical knowledge for nurses and healthcare professionals.
Importance of Monitoring Peripheral IV Therapy
Peripheral IV cannulas are placed into superficial veins, usually in the hands or arms. Because they provide direct access to the bloodstream, even minor complications can lead to significant patient discomfort, infection, or tissue damage. Regular assessment of the IV site helps in:
- Early detection of complications
- Prevention of severe tissue injury
- Ensuring uninterrupted and effective therapy
- Improving patient outcomes
Common Complications of Peripheral IV Therapy
1. Infiltration
Definition:
Infiltration occurs when non-vesicant IV fluids leak into the surrounding tissue due to displacement of the cannula from the vein.
Clinical Signs:
- Swelling at or around the IV site
- Skin feels cool to touch
- Pain or discomfort
- Decreased or stopped IV flow
- Blanching or tightness of the skin
Nursing Action:
Stop the infusion immediately, remove the cannula, elevate the limb, and apply a warm or cold compress as per institutional protocol.
2. Extravasation
Definition:
Extravasation is the leakage of vesicant (tissue-damaging) drugs into the surrounding tissue.
Clinical Signs:
- Severe pain or burning sensation
- Swelling and redness
- Blistering or skin necrosis (in severe cases)
- Sluggish or absent IV flow
Nursing Action:
Stop the infusion immediately, do not flush the line, notify the physician, and follow extravasation management guidelines specific to the drug.
3. Phlebitis
Definition:
Phlebitis is the inflammation of the vein caused by mechanical, chemical, or bacterial irritation.
- Clinical Signs:
- Redness along the vein
- Warmth at the site
- Pain or tenderness
- Palpable, cord-like vein
Nursing Action:
Remove the cannula, apply warm compresses, and document the findings. Restart IV therapy at a different site if required.
4. Thrombophlebitis
Definition:
Thrombophlebitis is phlebitis accompanied by the formation of a blood clot within the vein.
Clinical Signs:
- Swelling of the limb
- Severe pain at the IV site
- Redness and warmth
- Vein feels hard and cord-like
Nursing Action:
Discontinue IV therapy, elevate the limb, apply warm compresses, and inform the physician.
5. Infection (Local and Systemic)
Definition:
Infection can occur due to poor aseptic technique or prolonged cannula use.
Clinical Signs of Local Infection:
- Redness and swelling at the insertion site
- Pus or discharge
- Local pain and warmth
Clinical Signs of Systemic Infection:
- Fever and chills
- Increased heart rate
- Generalized weakness
Nursing Action:
Remove the cannula, send the tip for culture if indicated, start prescribed antibiotics, and maintain strict infection control practices.
6. Hematoma
Definition:
A hematoma is a collection of blood under the skin caused by vessel injury during insertion or removal.
Clinical Signs:
- Bluish or purplish discoloration
- Swelling
- Pain at the site
Nursing Action:
Remove the cannula, apply firm pressure, and elevate the limb.
7. Occlusion
Definition:
Occlusion occurs when IV flow is blocked due to clot formation or catheter kinking.
Clinical Signs:
- Resistance while flushing
- IV pump alarms
- Reduced or absent flow
Nursing Action:
Assess for kinks, reposition the limb, and remove the cannula if patency cannot be restored.
8. Fluid Overload
Definition:
Fluid overload results from excessive or rapid infusion of IV fluids.
Clinical Signs:
- Edema
- Shortness of breath
- Crackles on lung auscultation
- Increased blood pressure
Nursing Action:
Slow or stop the infusion, monitor vital signs, and inform the physician immediately.
Prevention of IV Therapy Complications
- Use proper aseptic technique during insertion and care
- Select the appropriate cannula size and site
- Secure the cannula properly
- Inspect the IV site regularly (at least once per shift)
- Educate patients to report pain, swelling, or discomfort
Conclusion
Peripheral IV therapy is an essential component of patient care, but it is not without risks. Understanding the common complications and recognizing their clinical signs early can prevent serious outcomes. Nurses play a vital role in ensuring safe IV therapy through vigilant monitoring, prompt intervention, and patient education. By following best practices, healthcare professionals can significantly reduce IV-related complications and enhance patient safety.

Hi, this is a comment.
To get started with moderating, editing, and deleting comments, please visit the Comments screen in the dashboard.
Commenter avatars come from Gravatar.
nLSSdUUmXUFAekcC
thc infused drinks enhance relaxation and creativity
Pingback: Choking: A Medical Emergency That Needs Immediate Action
Pingback: 4 Stages of bedsores its Nursing Management